Psilocybin’s Long-Term Reduction of OCD Symptoms
Obsessive-compulsive disorder (OCD) is a neuro-psychiatric ailment that is extremely common and incapacitating, for which the currently available treatments are insufficiently effective and alternative therapies deserve top emphasis.
Psilocybin may offer those suffering from this ailment a secure and efficient therapeutic option. This chapter provides a brief overview of the OCD symptoms, epidemiology, and pertinent disease-mechanism hypotheses that may help guide treatment decisions.
In order to prepare for the future use of psilocybin and maybe related substances in the treatment of OCD and associated diseases, we briefly discuss the currently available treatments, mechanisms of action, and efficacy limits. Although the mechanisms of action of psychedelic substances are extensively covered in this book, a specific examination of the effects of psilocybin on OCD is also provided.
Introduction
Obsessive Compulsive Disorder (OCD) is a persistent neuropsychiatric illness marked by obsessions and compulsions that typically interferes with a person’s ability to go about their daily lives.
- A lifetime prevalence of 2-3% is observed. About 41-43% of patients do not respond well to the first-line treatment.
The scientific literature contains case studies demonstrating a reduction in OCD symptoms following the use of psilocybin-containing mushrooms. In one case study, a patient with treatment-resistant OCD saw a long-term improvement in symptoms after eating psilocybin-containing mushrooms.
Mechanisms of Action (MOA): OCD
OCD is a diverse condition with several clinical subgroups that have been proposed, some of which have been linked to biological, psychological, developmental, and environmental risk factors as well as having unique disease trajectories and therapeutic responses.
It is safe to believe that there is no one disease mechanism that accounts for OCD, and the complexity of the OCD phenotype may account for at least some of the variation in results between studies using pharmacological, psychotherapeutic, imaging, genetic, epidemiologic, and other study methods.
Psychological Explanations: OCD
Obsessional neurosis, a term used before the modern OCD diagnosis, is thought to be the outcome of unresolved fixations or regressions to early phases of psychosexual development, notably the “Anal Phase,” according to traditional psychoanalytic ideas.
As conscience and cultural development take place, aggressive and sexual impulses clash with a rigid superego and some ego defences in the anal phase because they are incompatible with personal imperatives. The creation of a fractured or ambivalent self is the main emphasis of more recent formulations influenced by object relations theory.
- Patients struggle to incorporate negative attributes about themselves into a positive self-perception and feel threatened by ideas that they are bad, flawed, unpredictable, unmanageable, or immoral.
Current psychological best practices for OCD have been developed with the backing of cognitive behavioral theories. According to learning theory, a stimulus that is normally neutral (such as a perception or thought) might start to arouse anxiety when it is regularly offered alongside a painful or distressing event (obsession formation).
Compulsions are then created and maintained to engage in escape or avoidance activities in order to lessen the anxiety. The following incorrect beliefs have been identified as characteristics of OCD:
- Assigning circumstances with a low likelihood of hazard a high probability of danger
- Exaggerating the seriousness of predicted adverse effects
- Assuming that something is harmful if there is no proof that it is safe
The emphasis on incoherent and improperly integrated attributions of self and other is shared by contemporary cognitive-behavioral formulations and traditional analytical approaches.
Obsessions and compulsions can serve the purpose of diverting patients’ attention away from lingering conflicts, some of which may be brought to awareness during the psilocybin experience, and which may be an important target for the support and integration that occurs in the context of psilocybin sessions, regardless of the specific psychodynamic formulation.
Biological Explanations: OCD
It is well known that OCD is heritable; estimates from twin studies suggest that between 27 and 65 percent of the variation in symptoms may be hereditary in origin. OCD also runs in families and is seen in afflicted relatives four times more often than in the general population.
The heterogeneity of ascertainment methods used in research may help to explain the wide range of results because some subtypes of OCD are unquestionably more heritable, such as early onset OCD. In addition to specific components of the serotoninergic, glutamatergic, GABAergic, and dopaminergic systems, a number of neurotransmitters, neurohormones, and immunological changes have been offered as reasons for the symptom development and treatment response.
- The serotonin transporter and the serotonin 2A receptor genes, in particular, appear to be more prevalent in OCD patients, according to molecular genetic studies. Additionally, glutamate’s function in the neurobiology and pathogenesis of OCD is well established, while more study is needed on the potential benefits of using this neurochemical in treatment.
But given the seemingly selective pharmacological response to serotonin-acting substances, the reports of serotonin-related changes in the central nervous system, and other changes in peripheral markers of serotonin function in OCD patients, the serotonergic system is among the most widely supported. It’s interesting to note that in OCD patients who have recovered, laboratory-induced decreases in brain serotonin availability do not increase the symptoms of obsessive-compulsive disorder.
- Contrarily, serotonin boosting drugs trigger an immediate recurrence of OCD symptoms in people who have recently improved selective inhibition of serotonin subtype-2 receptors (5HT2).
- Atypical neuroleptics and mirtazapine, two commonly used 5HT2 blockers, also seem to be effective in the treatment of OCD. These results imply that the response to OCD involves complicated postsynaptic functional and anatomical changes that may affect the function of numerous neurochemicals, regions, and/or circuits rather than just activation at a single receptor.
Neurological Explanations: OCD
Initiation and termination of thoughts and behaviors are governed by parallel and partially segregated circuits, according to data from animal models and functional and structural human brain imaging investigations.
- The so-called Cortico-Striato-Thalamo-Cortical (CSTC) circuit describes the connectivity between the thalamus, caudate nucleus, and orbitofrontal cortex; nevertheless, a broader number of areas often interacting with CSTC have been linked to OCD.
It’s interesting to note that some OCD symptom dimensions seem to be linked to discoveries in various brain regions, further proving the disorder’s heterogeneity.
The proposed OCD corticostriatal hyperactivity results in a persistently high error signal, which in turn causes its hallmark psychopathology, including irrational fears or obsessions, or that an action was not performed correctly in accordance with a set of internal unattainable rules, which sets off repetitive, compensatory behaviors (i.e., compulsions). The amplitude of this error signal’s index, which varies according to the degree of OCD symptoms, is higher in OCD patients.
Treatments
Pharmacotherapy
The use of Cognitive Behavioral Therapy (CBT) for OCD is supported by current treatment guidelines, with an emphasis on the need of Exposure and Response Prevention (ERP) and/or prescription using serotonin reuptake inhibitor drugs.
Only a few treatments for this illness have received FDA approval in the United States. The following are examples of powerful serotonin reuptake inhibitors that improve serotonin function:
- Clomipramine (Anafranil®),
- Fluoxetine (Prozac®),
- Fluvoxamine (Luvox®),
- Sertraline (Zoloft®),
- Paroxetine (Paxil®)
Despite their proven effectiveness, a number of drawbacks prevent them from fully enhancing a patient’s performance. For instance, only about half of patients receiving adequate treatment-trials will achieve a satisfactory response, and the majority of patients who do improve only have a one-third to one-half decrease in severity ratings. This is despite the fact that OCD medications are frequently prescribed at higher doses and for longer periods than for other disorders. Their lingering symptoms keep them from functioning normally and make them more susceptible to problems and exacerbations.
OCD has been shown to be unresponsive to medications like desipramine and bupropion, which may work largely by improving norepinephrine and/or dopamine function. Serotonin-related therapy alternatives should be investigated in this population due to the apparent selectivity of treatment response to medicine that operates on the serotonin system and the observation that serotonin blockers result in a return of OCD symptoms.
Psychotherapy
The cornerstone of non-analytic therapy and the first option for treating OCD is CBT. CBT consists of two parts: a behavioral intervention to stop symptom engagement and a cognitive reassessment of incorrect beliefs. The preferred treatment for OCD is ERP, which entails exposure to fear-inducing stimuli over a long period of time while also giving instructions to refrain from the compulsive activity.
- For patients with limited insight or those who would find exposure treatments difficult to stomach, the combination of ERP with cognitive components, such as the discussion of feared consequences and other dysfunctional beliefs, can improve the acceptability and effectiveness of ERP.
Treatment Options for Non-Responsive Patients
The best results often result from a mix of these treatment types, even if both medication and psychotherapy can be helpful individually (pharmacology and CBT). After adequate trials of evidence-supported first line interventions, if these treatments are found to be ineffective due to intolerance or lack of benefit, an increasingly complex series of alternatives may be considered, frequently with the intention of reducing symptom severity rather than aiming for symptom remission.
These include the use of deep brain stimulation (DBS) in the anterior cingulate cortex and other targets, electroshock therapy, alternative pharmacological trials, augmentations, and combination techniques, as well as surgical ablation such as cingulotomy and other lesion-based therapies.
Only in patients with severe treatment resistance that have exhausted all other alternatives may surgical procedures be considered.
- Finding new treatment options for patients with severe and treatment-resistant OCD has become a top priority because a sizable portion of people continue to experience symptoms and impairment despite the use of more aggressive treatment strategies, which are associated with increased morbidity and a decreased likelihood of benefit.
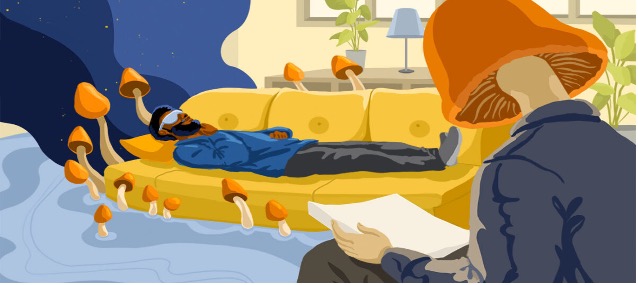
Psilocybin for OCD
Although psilocybin, LSD, and mescaline have been found to bind to several receptors, transporters, and other proteins, their extraordinary efficacy as agonists at the 5-HT1A, 5-HT2A, and 5-HT2C receptors is directly connected with their potency as hallucinogens in humans.
- The initial improvement in symptoms described in the published case reports may be explained by the participation of other sites of action, although it is likely that interactions with the 5-HT1A, 5-HT2A, and 5-HT2C receptors play a significant role in anti-OCD medication action. Increases in postsynaptic 5-HT1A activation and long-term 5-HT2A reduced expression are caused by SSRIs.
The aforementioned reports raise significant concerns, such as why psilocybin’s anti-obsessional effects are so quick while those of powerful serotonin enhancers like clomipramine and SSRIs take weeks to months to manifest their therapeutic effects.
Over the past two decades, research on OCD, psychedelic mechanisms, and brain circuitry has advanced, raising the possibility that a more complicated mechanism than that initially hypothesized is at work. This mechanism may involve a number of postsynaptic effects, interactions with other neurochemical systems, and brain circuits involved in the anti-obsessional response.
Researchers have hypothesized that serotonin neurotransmission promotes two distinct adaptive responses to adversity, where postsynaptic 5-HT1A signaling mediates passive coping characterized by stress moderation (SSRI treatments) and 5-HT2A signaling promoted by psychedelics mediates active coping and further enhances plasticity.
- The failure of metabotropic glutamate receptor-2 (mGluR2) knockout animals to exhibit cellular and behavioral responses to LSD comparable to 5-HT2A knockouts suggests that the interaction of mGluR2 and 5-HT2A is required for the occurrence of certain neuro-behavioral consequences.
A disruption of the CSTC circuits may be a good target for the treatment of OCD with psychedelics, as evidenced by the normalization of CSTC circuits in individuals with OCD following successful treatments, including both pharmaceutical and psychosocial therapies. In sensorimotor and ventral cognitive networks, patients with OCD have stronger functional connection and ventral striatal activity, whereas dorsal striatal circuits exhibit lower functional connectivity and disinhibition.
Psilocybin Efficacy for OCD
Psilocybin has been linked to a change in neocortical 5-HT2A receptor binding followed by long-term improved mindfulness, offering another perspective on its possible therapeutic advantages. It has also been demonstrated that 5-HT2A signaling can improve neuronal plasticity, low-level learning, and extinction learning, which is a crucial element of ERP and CBTs in OCD.
Additionally, psychedelics may stimulate DMN neuroplasticity. If the DMN is in control of information integration, it stands to reason those current narratives, which in the case of OCD might be described as rigid and overlearned thought patterns and beliefs, will disregard incongruent or dissonant information resulting from perceptual abnormalities and ambiguities.
- It is believed that psychedelics obstruct this limiting mechanism. By interrupting and “resetting” the DMN, one can loosen the excessive self-referential cognitive activity that is typical of OCD. This promotes a better interaction with the world and breaks free from strict top-down information processing patterns.
Therefore, a variety of levels of analysis encourage hope regarding the use of psychedelics to alter rigid patterns in OCD, both neurological and psychological.
- There is enough evidence to support the use of the psychedelic class of drugs as a means of quickly reducing OCD symptoms, with the clinical benefit lasting significantly longer than the subjective effects of the drug, opening the door for significant investigations of therapeutic potential, regardless of the level of analysis one prefers to describe the potential mechanism of action.
Conclusion
When given in a welcoming clinical setting, psilocybin is widely accepted and temporarily relieves OCD symptoms. Psilocybin and other psychedelic drugs have the potential to be used in the future as a treatment for a variety of mental diseases, especially those characterized by rigid, repeating negative thought patterns and the inability to control undesirable behaviors.
Psilocybin may be a significant agent to pursue as we look into other OCD therapy options, according to preliminary evidence.
- Additionally, the potential of utilizing psychedelics as part of an intervention strategy for those with treatment-resistant OCD is further motivated by the current research foundation regarding brain chemistry and network function in OCD and how patients respond to the administration of psychedelics.
The CSTC circuits are hypothesized to be disturbed by the 5-HT2A agonism of psychedelics. It has been suggested that this disruption reduces the thalamus’ filtering of sensory input, allowing more information to reach the cortex.


